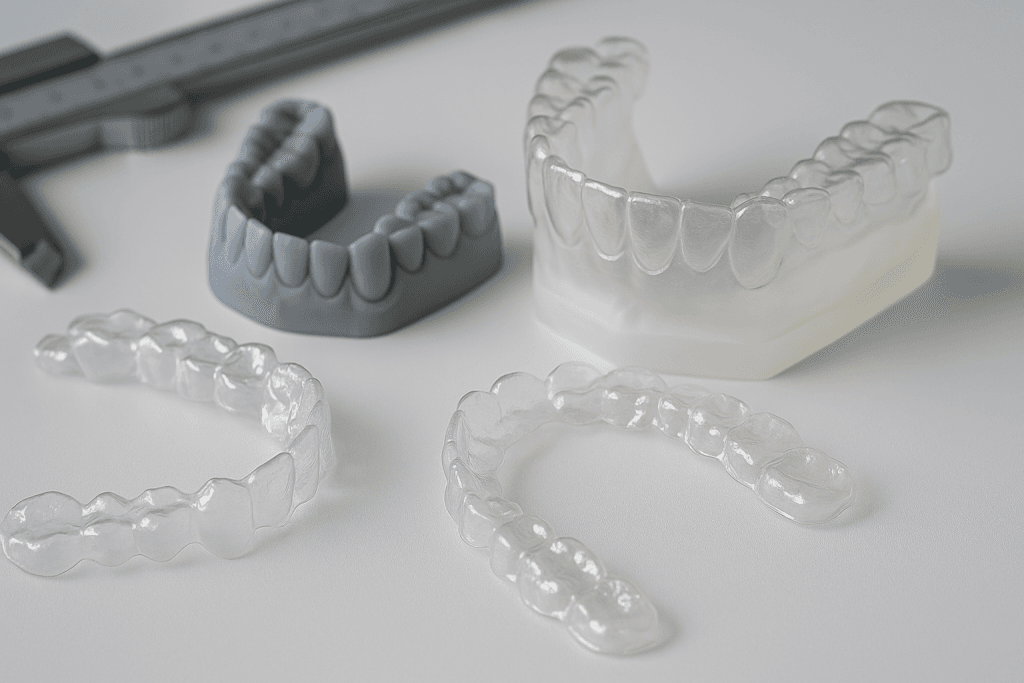
Clear aligners look simple from the outside, but building a truly premium product is an exact science. The difference shows up in comfort, clarity, tooth-movement accuracy, breakage rates, turnaround time, and even how consistently each tray in a series performs. Below is a practical, inside-the-manufacturing unit look at the quality controls that separate top-tier manufacturers from the rest.
1) Material Science That’s Proven—Not Just Promised
Medical-grade polymers & multi-layer films. Premium aligners start with certified, medical-grade thermoplastic polyurethane (TPU) or co-polyester—often in multi-layer stacks designed to balance elasticity, crack resistance, and stain resilience. Materials are sourced with Certificates of Analysis (CoA) and lot traceability so any roll can be tracked back to its supplier and test results.
Biocompatibility & stability testing. Reputable clear aligner manufacturing companies validate materials against ISO 10993 and conduct migration/extractables tests, saliva/temperature aging, and force-retention over time. They also test optical clarity and scratch resistance, because dull or cloudy trays often indicate inconsistent resin, overheating, or poor polishing.
Tightly controlled thickness. Force delivery depends on thickness. Premium plants verify sheet thickness in multiple zones (using calibrated micrometers and SPC charts) before thermoforming and after trimming to keep aligners within a narrow tolerance band—commonly ±0.05 mm or better.
2) Precision at Every Digital Step
Scan quality gate. Great manufacturing starts with accurate inputs. Top manufacturers run pre-production scan checks: resolution, holes, cross-arch alignment, and bite registration. Cases that don’t meet criteria are flagged early, avoiding downstream errors.
CAD treatment planning with peer review. Treatment plans aren’t just technician-led; there’s a clinical protocol with automated movement limits (IPR, attachments, extrusion/intrusion ranges) and human review for edge cases. Senior planners or orthodontists sign off on complex movements, Class II/III strategies, and root positioning.
Printer calibration & model integrity. 3D-print dental models, XY and Z calibration are checked daily (test coupons), supports and model orientation are standardized to reduce warping, and resin post-cure is time- and temperature-controlled. Warped models = poor aligner fit.
Closed-loop nesting rules. Model layout, margin offsets, and trim paths are standardized and saved to SOPs so repeat orders behave the same way across batches and printers.
3) Thermoforming Done the Right Way
Validated temperature profiles. Overheating can collapse detail, and underheating causes weak forming. Premium lines validate heater temperature, dwell time, and vacuum pressure by material type, with log sheets and alarms on the machine HMI.
Tooling consistency. Forming platforms are cleaned and inspected between cycles. Anti-static handling reduces dust inclusions that can cloud a tray.
In-process checks. Operators inspect draw depth, detail capture in undercuts, and edge uniformity on the line. Anything borderline is held in quarantine for a supervisor check—no exceptions.
4) Trimline, Edges, and Finishing That Patients Feel
Trim accuracy. Whether scalloped or straight-line, the CNC trim path must match the planned margin. Variations cause sore spots or reduced retention. Premium aligner manufacturers verify trimline offset on random samples per shift.
Smooth, sealed edges. Polishing is not cosmetic—it’s comfort and tissue health. Premium workflows use multi-stage deburring, micro-polishing, and final visual inspection under bright, angled light to catch micro-burrs. Rough edges are a leading cause of patient complaints; great engineer them out.
5) Cleanroom Hygiene and Safe Handling
Controlled environment. High-end manufacturers run final assembly in ISO-classified clean zones with HEPA filtration. Operators wear gloves and hair covers; trays are handled with minimal contacts to avoid micro-scratches and contamination.
Sanitization & packaging validation. Pouches, inserts, and boxes are food/medical-grade and lot-tracked. Some brands validate sterility assurance for specific workflows, or at minimum use validated cleaning protocols that leave no residue or odor.
6) Traceability, Labels, and Serialization
UDI/serialization. Each tray is serialized with patient ID, stage number, arch, and production lot etched or printed (without weakening the tray). That data links to the full Device History Record (DHR)—machines used, operators, material lots, and QC sign-offs.
MES that actually works. Premium plants run a Manufacturing Execution System so every step—from material release to final packing—is timestamped. If an issue is reported, the manufacturing team can pull the exact lot, shift, and machine parameters in minutes.
7) Certifications and Audit Readiness
Quality system standards. Look for ISO 13485 for medical devices, plus market-specific compliance (e.g., FDA registration/510(k) where applicable, EU MDR, MHR UK/CE, TGA, etc.). More than a logo, this means documented SOPs, competence records, calibration logs, and CAPA (Corrective and Preventive Action) discipline.
Supplier audits. Premium brands audit material suppliers for change control, consistency, and contingency planning. When a supplier changes a resin backbone or film lamination method, the manufacturer triggers re-validation before rolling it into production.
8) Testing That Predicts Real-World Performance
Fit and retention tests. Random trays are seated on master dies with pull-off force measured to ensure consistent retention ranges.
Stress and fatigue. Mechanical testing simulates chewing and insertion cycles to observe crack initiation and edge chipping. Results feed back into trim strategies and edge radii.
Stain & odor resistance. Tea/coffee/colored-dye baths and halitosis simulations help validate cleaning guidance and material selection.
Force-delivery curves. The gold standard is verifying that the tray applies the intended force at the intended point in the movement. Top manufactureres test this during product validation and after any process change.
9) On-Time, In-Full—Without Cutting Corners
Turnaround with controls. Speed matters, but not at the expense of predictability. Premium setups use capacity planning, buffer stock for critical materials, and bottleneck dashboards so urgent cases don’t derail the line.
Right-first-time KPIs. Watch remake rate, on-time-in-full (OTIF), and average days per refinement. Consistently low remake rate is a strong proxy for stable upstream processes.
10) Feedback Loops With Clinics
Proactive case monitoring. Great manufacturers look at non-tracking patterns (e.g., specific movements, tooth types, or attachments) and update planning protocols. They also share clear clinician guidance on wear schedules, chewies, and tray care to protect outcomes.
Fast, fair remakes. When refinements are needed, premium partners respond quickly with documented root-cause analysis—was it scan quality, plan, forming, trim, patient wear, or attachment bonding? This transparency builds trust.
11) Sustainability Without Surprises
Waste minimization. Optimized nesting, material off-cut recycling where regulations allow, and energy-efficient curing/heating reduce footprint.
Responsible disposables. Packaging is sized right, inks are low-VOC, and documentation moves digital wherever possible.
A Simple QC Checklist for Clinics to Ask Manufacturers
- Materials: Medical-grade? Multi-layer? Biocompatibility reports and CoAs on file?
- Digital controls: Scan acceptance criteria, peer-reviewed planning, printer calibration logs?
- Forming & finishing: Validated temperature/pressure; edge polishing SOP with inspection records?
- Cleanliness: Controlled environment for final handling and packing?
- Certifications: ISO 13485 and relevant market approvals current?
- Testing: Force-delivery validation, stain/fatigue testing, retention tests performed?
- KPIs: Current remake rate and OTIF stats?
- Support: Clear remake policy and clinical support response times?
Final Word
Premium clear aligners don’t happen by chance—they’re the result of disciplined systems, validated materials, skilled people, and constant feedback from clinics. When those pieces are in place, patients feel the difference: better comfort, more predictable tooth movement, fewer refinements, and a smoother journey from first tray to final smile.